Prescribing opiates in non-cancer patients
About the project
The National Medicines Safety Improvement Programme (MedSIP) aims to help patients get the maximum benefit from their medicines and reduce waste with an overarching aim to reduce medication related harm in health and social care, focusing on high-risk drugs, situations, and vulnerable patients.
NHS England and Improvement launched MedSIP as part of the National Patient Safety Strategy and it is delivered locally by the West Midlands Patient Safety Collaborative (WMPSC).
Project ambitions
The programme will contribute to the World Health Organisation (WHO) third global safety challenge. The overarching aim of MedSIP is to reduce severe avoidable medication-related harm by 50% by March 2024. To do this we will be focusing on improving the care of people living with chronic non-cancer pain, by reducing harm from opioids.
Our local delivery will focus on improving the care of people living with chronic non-cancer pain, by reducing the prescribing of high-risk opioids.
Why is this a focus?
Opioids are a highly effective class of analgesics and, when used judiciously, are of great benefit to many people living with pain.
In 2019 a review by Public Health England shows that from 2017 to 2018, 540,000 adults in England were prescribed opioid pain medicine for three years or more.
The Faculty of Pain Medicine has advised that increasing opioid load above >120mg/day morphine equivalent is unlikely to yield further benefits but exposes the patient to increased harm.
National Institute for Health and Care Excellence (NICE) guidance published in March 2021 recommends that opioids should not be initiated to manage chronic primary pain in people aged 16 years and over.
The effects of COVID-19 are anticipated to have exacerbated the use of opioids for chronic pain, which is linked to both deprivation and the prevalence of mental health conditions such as anxiety.
Management of chronic non-cancer pain requires personalised care and shared decision making at its core, with patients also requiring biopsychosocial support so that they can live well with pain.
National ambitions
The national ambition for 2022-23 is to reduce harm from the prescribing of oral or transdermal opioids, (of any dose), for more than three months in chronic non-cancer pain by end of March 2023.
The West Midlands will collectively contribute to these ambitions:
- 30,000 fewer people prescribed oral or transdermal opioids, (of any dose), for more than three months, preventing approximately 484 deaths
- Of the 30,000 above, 4,500 of these will have been prescribed a high dose opioid (>120mg day Morphine Equivalent) and have now stopped opioids, preventing 500 hospital admissions, and saving around £1.75m in admissions costs
The WMPSC will support at least one Integrated Care System (ICS) to design, develop and implement a system wide improvement programme focussed on those at risk of becoming dependant, and reducing the risk in those who could be considered dependant on opioids.
A framework has been developed following a national ‘real world’ study of interventions aiming to reduce harm from opioids. This seven-phase framework is a whole systems approach to reduce high-risk opioids prescribing, contributing to achieve this national ambition.
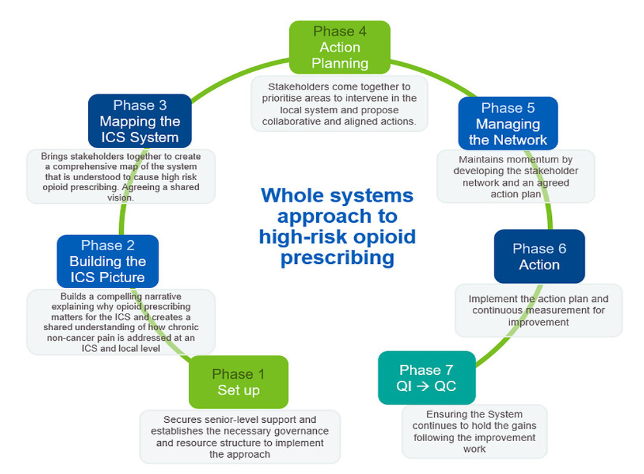
- Phase One: Set up
- Phase Two: Building the ICS picture
- Phase Three: Mapping the ICS system
- Phase Four: Action Planning
- Phase Five: Managing the network
- Phase Six: Action
- Phase Seven: QI to Quality Control (QC)
Work undertaken will be underpinned by the principles of QI, co-designed with patients/the public and patient safety learning.
Resources to support
- The detail of this approach, plus supporting background information, can be accessed through FutureNHSworkspace
- To learn how to use the Opioid Comparators on the NHS Business Services Authority (NHS BSA) Opioid Dashboard watch this video
Find out more
Get in touch with a member of the project team below to find out how you can get involved.
- Caroline Maries-Tillott, Assistant Programme Manager: caroline.maries-tillott@healthinnovationwm.org
