Medicines Safety Improvement Programme 2021/22 (MedSIP) – PROJECT CLOSED
About the programme
The Medicines Safety Improvement Programme (MedSIP) aims to help patients get the maximum benefit from their medicines and reduce waste. The overarching aim is to reduce medication related harm in health and social care, focusing on high risk drugs, situations and vulnerable patients.
Each area of work in this programme intends to make medicines safety part of routine practice, to ensure medicines use is as safe as possible and understand the patients’ experience.
Medicines administration in care homes
As part of the national medicines’ safety programme 2021/22, West Midlands Health Innovation Network (formerly known as the Health Innovation West Midlands) worked with care homes staff to reduce and avoid harm arising from medicine administration omissions errors and delays.
This work was part of a national Medicines Safety Improvement Programme (MedSIP) to reduce severe avoidable medication related harm by 50% by 2024.
To contribute to this ambition, by March 2022, Patient Safety Collaboratives across England have focussed on five defined interventions (see the secondary drivers in the Medicines Safety Improvement Programme Driver Diagram below) that had potential to both improve patient safety in care homes and be implemented at a national scale in order to improve the safety of medicines administration.
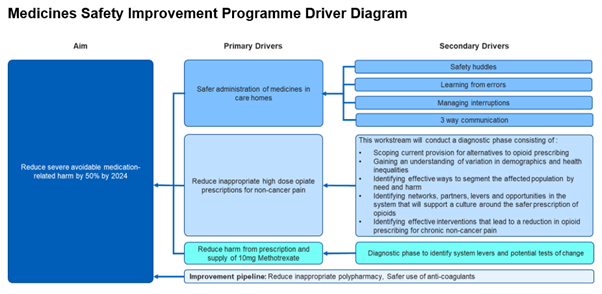
HIWM focussed on three of the five secondary drivers, namely learning from error and managing interruptions.
Summary of QI work relating to Interruptions:
HIWM has designed and tested several interventions to reduce the number of interruptions to medicine rounds in three care homes.
Care Home 1 exceeded the overall aim. Results showed a significant and sustained reduction in interruptions and reduced the mean number of interruptions from 3.45 to 0.87 per medicine round. This represents a 75% reduction in interruptions.
Care Home 2 also demonstrated significant reductions in interruptions with 44% and 50% reduction in the nursing unit and residential units, respectively.
Findings from the baseline audit in a third care home (a small mental health care home) demonstrated that the number of interruptions was not significant enough to warrant a QI project (1-2 interruptions per day).
Conclusion
HIWM has shown that care homes can deliver significant reductions in interruptions to medicine rounds using QI methodology. It is possible that those interventions that demonstrated most significant impact in reducing interruptions could be disseminated. However, without the structured QI approach to delivering improvements including the collection, analysis and review of data and staff engagement, these impacts are likely to be limited and not sustained.
The support required for this to be implemented at a national scale is significant. Careful consideration is needed regarding the return on investment to achieve large scale adoption and spread.
A report outlining the reductions to the medicine round interruptions QI project in a Birmingham Care Home featured in Care Management Matters journal titled Finding new ways to improve medicine administration in care homes | CMM
Learning from incidents
HIWM also designed and tested the learning from incidents intervention in two care homes in the West Midlands region. HIWM identified that there is significant under-reporting of medication incidents in care homes. This finding has been acknowledged by other Health Innovation Networks working on this secondary driver and by the CCGs who support care homes.
The WMPSC identified multiple reporting routes for care homes in relation to medicines incidents. Current under-reporting (hidden iceberg) represents a risk to resident safety in care homes as it does not reflect the current incident rate and precludes opportunities for learning. There would appear to be several barriers to learning from incidents; most (but not all of which) relate to medicines incident reporting per se:
- Lack of understanding of what constitutes a medication incident, error or near miss.
- Lack of clear reporting guidance for incidents – except for severe incidents that require reporting to CQC and Safeguarding, there is lack of clear guidance from CCGs available to care homes about which organisation(s) and how, to report low harm and near miss incidents to and yet these have significant potential for system wide learning.
- Lack of clinical I.T. infra-structure in smaller care homes providers to capture medicines incidents and generate themes and trends for potential learning.
- Lack of psychological safety – fear of consequences of reporting incidents.
- Dominance of Safety-I approach (reactive) vs Safety-II culture (proactive).
- Care home resource – care home staff are overburdened, and turnover is high amongst managers and staff. Staff tend to focus on resolving incidents and preventing potential harm rather than reporting incidents.
- CCG resource – if there was a significant increase in reporting medicines incidents from care homes, it is unclear if the CCGs or PCNs have capacity to support learning.
Conclusion
It is difficult to see how the above barriers will be resolved easily. Indeed, potential intervention from regulators may help but only if an understanding of Safety II culture is inherent within the approach. It is also difficult to see how the new national Learning from Patient Safety Events service will address this in the near future for care homes as it is still in the early stages of roll out.
A recent development with one CCG to increase medicines incident reporting and subsequent learning in multiple care homes is more promising. This approach has more potential for extensive scale-up across ICS settings. The leadership, direction and influence provided by the CCG increase the likelihood of this being a more sustainable approach.
Safety champions
To develop and test the concept of Medicine Safety Champions, HIWM worked with 8 Medicine Safety Champions (MSCs) in two care homes in the region.
WMPSC successfully assessed the confidence of the MSCs at three stages of the QI project (Before, Mid-point and End) to improve safety in their care home. At each stage, HIWM assessed the MSCs confidence ratings as they progressed with their QI project. Six out of the seven MSCs reported a significant improvement in their confidence to improve safety in their care homes.
Conclusion
The concept and roll out of Medicine Safety Champions have potential for care homes however, HIWM experienced ongoing issues relating to understaffing and interdependencies such as the pandemic. This meant that MSC’s work was not always a priority. The MSC model would benefit from an ongoing “train the trainer” model with resource to support this.
Current work
NHSE/I commissioned Medicine Safety Improvement work in care homes concluded in 2023. HIWM is currently working on the National MedSIP programme
There are two elements to this programme: Reducing harm from opioids in managing chronic non-cancer pain; and optimising the use of psychotropics in people with learning disability and of medicines for frail patients that may induce falls.
Find out more
For more information contact a member of the programme team below:
- Caroline Maries-Tillott, Assistant Programme Manager: caroline.maries-tillott@healthinnovationwm.org
- Claudia Li, Assistant Project Manager: claudia.li@healthinnovationwm.org
- Jodie Mazur, Associate Director Implementation & Improvement: jodie.mazur@healthinnovationwm.org
