Lessons from HETT North 2025
By Hayley Jary, Digital Marketing Coordinator, Health Innovation West Midlands
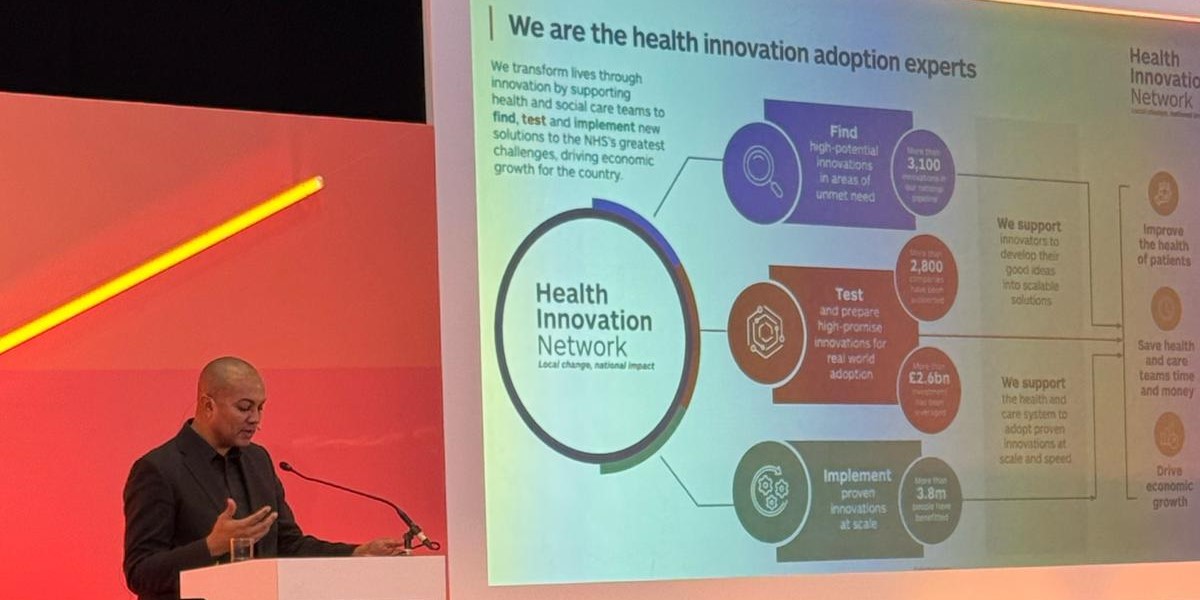
Putting innovation at the heart of the three big shifts in healthcare is essential to success. This was the key message from the Chair of the Health Innovation Network, Richard Stubbs, during his keynote address.
Other themes from the day include the importance of patient engagement in the innovation process, ensuring their voice and experience is heard, and a need for standardised pathways into the NHS for innovators, with clear communication throughout the journey.
Digital health innovation – An engine for health and growth
Richard Stubbs discussed the transformative impact of digital health innovation across the UK and stressed that innovation must be at the core of all three of the NHS big shifts – moving care from hospitals to the community, embracing digital transformation, and shifting from treatment to prevention.
As the innovation arm of the NHS, the Health Innovation Network are experts at adopting, adapting and embedding innovations to improve health and generate economic growth. Richard stated that improving population health will boost the country’s GDP, which in turn improves our wealth and prosperity.
He also gave a sneak peek at the Network’s seven conditions for scaling and embedding innovations which includes, thinking about pathways not products, building coalitions not concerns and linking policy to problem solving.
If you are an innovator wondering how to get the decision makers in NHS, contact your local Health Innovation Network. We are inputting into the NHS 10 year plan and trying to implement ways to make it easier for social enterprises and SMBs to get their innovations rolled out at pace and scale.
Innovation without boundaries – Building a scalable, financially supported and modern NHS
This panel session discussed what needs to be in place to enable innovation in the NHS to flourish and scale in a way which is necessary to improve outcomes, and the barriers that currently hinder this progress.
Small and medium-sized businesses often face obstacles when trying to engage with the NHS because, as Ian Hogan, Chief Digital Information Officer at Leeds and York Partnership NHS Trust, points out, the NHS is like a franchise, each trust can have different rules/criteria for submitting an innovation.
Dace Dimza-Jones, National Life Sciences Inward Investment Specialist at the Department for Business and Trade, spoke about the need to know how to navigate the NHS and how to get access to funding. “Standardisation across trusts is needed, as current processes discourage innovators from abroad.”
She also highlighted that there is a need for clear messaging to innovators of the needs of each region, so that they can save time and target their efforts accordingly. Communication needs to improve between the NHS and innovators, processes can sometimes take time, but if the answer is no, this needs to be communicated more quickly.
The patient perspective was represented by Olivia Burns, a Patient Entrepreneur from the NHS Clinical Entrepreneur Programme. Olivia talked about how patients need to be listened to more. They have an inside view of the patient journey from start to finish and can give important insight to current processes and make suggestions for improvement. Patients need to be more involved in their care and PPIE needs to be integrated more into the NHS.
Dace seconded this and has noticed that patient empowerment is more prevalent in other countries. She says we should be encouraging patients to be more vocal as they want to be part of trials and have access to innovations.
Olivia also suggests there needs to be a cultural change to innovation, using the infrastructure already in place, but public and private organisations need to work together. “Private companies have the time and resources to deliver, the NHS needs to let them in.”
Andrew Davies, Digital Health Lead at ABHI, spoke of the need for a view of the whole system clinical care pathway, as different trusts have different KPIs and interests. Clinicians are interested in innovation and it is encouraged from the top level, but progress is being stalled.
He says that one of the major obstacles is procurement. “There needs to be more focus on long term investment. Look at what you’ll get out of it. The impact and the value. There is a risk to keep buying the lowest cost thing, but it’s not necessarily the best value and delivering the best outcomes.”
Nicholas Appelbaum, Co-Founder and CEO at Dosium, agrees that to encourage front line innovation, procurement needs to be more accessible. He says, the NHS has a high risk tolerance in terms of its day to day activity, the work it does has consequences, but in terms of innovation it is not being ambitious enough. “Disruption is disruptive, innovation is change, change is difficult.”
Ian Hogan points out that this is because the NHS is risk averse as it is scared of making mistakes, but it must share and collaborate more and allow clinicians time to innovate, as without innovation the NHS will regress.
So, how do you remove the barriers to getting innovations into the NHS? Contact your local Health Innovation Network. The HINs work closely with their local ICSs and NHS Trusts to determine their needs and to bridge the gap between the NHS and innovators, making the process smoother and easier to navigate.
If you are an innovator in the West Midlands, or are looking to introduce your innovation to our region, please get in touch to find out how we can help: discover@healthinnovationwm.org
