Welcome

It is with immense pleasure that we introduce our annual Impact Report.
2023 marked an important milestone for the Health Innovation Networks nationally, with the Government and NHS England’s decision to relicense England’s 15 Academic Health Science Networks for a further five years. We are now looking to advance the successes achieved as an Academic Health Science Network under the new banner of Health Innovation Networks.
The new name reflects our vision to transform local health and care through collaborative innovation. Working with integrated care systems, innovators, researchers and health and care systems, HIWM will continue to develop solutions and innovations meeting local need, as well as accelerating the adoption and spread of proven solutions.
The healthcare sector continues to be a highly dynamic and evolving environment, with several changes across the landscape during 2023-24. The West Midlands has the fastest growing population in the UK, which has seen an increase by 40,000 in the last year, remaining the second largest population in the UK.
As an organisation, we continue to work closely and collaboratively with our commissioners – NHS England, NHS Improvement, and the Government’s Office for Life Sciences, as well as strengthening our partnerships with organisations like the NIHR Applied Research Collaboration West Midlands (ARC WM).
Our Overall Impact
Case Study Spotlight
Polypharmacy

Polypharmacy simply means many medicines. Every year, the primary care sector in England dispenses over 1 billion prescription items. As more people are living longer, the number of patients managing multiple long-term conditions also increases. This can have a significant burden on the patient, as they are navigating multiple medicine regimes which could, if combined wrongly, be harmful.
Studies have shown that over 50% of older people are prescribed a medicine that is causing more harm than benefit. This is resulting in avoidable morbidity, hospitalisation and excess mortality for patients, while also contributing to preventable costs to the healthcare system. A person taking ten or more medicines is 300% more likely to be admitted to hospital. The most deprived areas tend to have the most issues around polypharmacy, also making this a health inequality issue.
Most of the harm from polypharmacy is preventable.
The Health Innovation West Midlands (HIWM) Polypharmacy Programme aims to support primary care to address problematic polypharmacy by using data to identify patients at potential risk of harm and support better conversations about medicines.
The project set out to support professionals limit the prescription of conflicting, or unrequired medicines, to help improve the safety of patients while reducing preventable costs.
The Polypharmacy Programme set out to manage the prescription health of patients by using data to understand their health risks and support the prioritisation of those most at risk by providing a structured medication review.
The primary care workforce was given training to develop their confidence in reviewing complex medicine regimes and de-prescribing where appropriate, through free, centrally run, Polypharmacy Actioning Learning sets, and locally run virtual Polypharmacy Workshops administered by HIWM.
A focus group was set up to gather patient opinions on public-facing materials, alongside a pilot study within primary care networks (PCNs) which trialled the materials during structured medication reviews and obtained feedback from clinicians and patients.Through this testing and evaluation process, the roll-out of public-facing materials led to public perceptions of prescribing medications being challenged and changed, and patients were encouraged to talk about medicines.
The NHS Business Services Authority webinar empowered 75 attendees with insights into identifying patients vulnerable to problematic polypharmacy, utilising polypharmacy comparators.
Through collaboration with HIWM analytics, three tailored data dashboards were crafted, prompting five integrated care boards (ICBs) to designate polypharmacy as a focal comparator. Concurrently, five local trainers achieved accreditation to facilitate polypharmacy education sessions, while nationally, 68 individuals engaged in Polypharmacy Action Learning Sets.
Moreover, 144 participants benefited from virtual workshops in the West Midlands. Three community of practice sessions were convened, attracting 119 attendees from a range of sectors.
Five clinicians completed Polypharmacy Quality Improvement projects, culminating in the publication of their work on the Health Innovation Network’s online library, with one project earning a prestigious PrescQIPP gold award.
Additionally, 55 downloads of the ‘Preparing for medication review’ patient pack were recorded, with feedback indicating intent by 73 primary care clinicians to integrate these materials into their practice. This effort is further supported by the incorporation of patient materials into local ICB structured medication reviews best practice guidance by the ICB Medicines Optimisations team.
Induction of Labour Support

The number of women having their labour induced has increased from 25% to 33% over the last ten years. This increase adds substantial pressure on UK maternity units. Locally, Birmingham Women’s Hospital (BWH) highlighted this as a particular area of concern.
During a one-week sample taken at BWH, 22 women were delayed in admission to hospital and 32 women were delayed in being transferred to a delivery suite. Initial data also identified a correlation between delays and poor outcomes for either mum or baby.
In response to this, the Health Innovation West Midlands (HIWM) Patient Safety Collaborative team, invited applications for funding of up to £20,000 to implement an innovation, or improvement intervention, that would result in improved outcomes for patients.
The aim of the fund, was to improve the experience and clinical outcomes for both the birthing parents and their babies, reducing delays and improving patient flow through the maternity unit.
Targets included:
- Increasing the percentage of women admitted for induced labour when required
- Reducing the number of women delayed by at
least 10% - Increasing the percentage of women transferred to the delivery suite within six hours
- Reducing the number of complaints by 50%
- Reducing the number of incidents resulting in harm from induction of labour (IOL) delays by 50%
- Increasing the overall percentage of data compliance
The fund enabled BWH to trial the implementation of a specialist IOL role. The IOL Flow and Capacity Coordinator was tasked to establish a more effective oversight and management process in the unit, which included the adoption of an electronic system for reviewing patient lists.
During the trial a Flow and Capacity Midwife was introduced alongside the Coordinator, to provide further specialist support. Thanks to the positive impact, a second fixed term midwife was also hired to ensure cover seven days a week.
The introduction of safe gestational ranges within the unit further helped to manage patient’s expectations,
and flow into the induction service, further reducing admission delays.
Applied across all inductions at BWH, the initial three-month trial supported an average of 58 women undergoing inductions per week. Within two years of the implementation of the role, delays in admission were reduced from over seven hours to just under 15 minutes. A business case has been submitted to extend the IOL Coordinator support to cover the unit 24/7.
The total length of time from IOL admission to birth was reduced by 16:05 hours, which improves outcomes for both parent and child. The percentage of women transferred to the delivery suite, receiving induction within six hours, increased from 43% to 57%.
As the national conversation around the need for improvement projects in IOL pathways has ramped up, BWH continues to provide information and resources highlighting best practice to other maternity units nationwide, to support tackling common problems and improve quality of care.
Heart Failure

Heart failure (HF) affects around 900,000 people in the UK, and this number is likely to rise, due to an ageing population, more effective treatments, and improved survival rates after a heart attack. HF is a large burden on the NHS, accounting for 1 million bed days per year, 2% of the NHS total, and 5% of all emergency admissions to hospital. (NICOR (2021), Heart Failure Audit 2021 summary report).
Despite advances in treatment, mortality remains high with around 30-40% of patients dying within a year of diagnosis.
Health Innovation West Midlands (HIWM) recognised that there is a wide variation in timely access to diagnostics and treatment, resulting in sub-optimal treatment. The HF project sought to address the pinch points within the clinical pathway that can be improved, either through education, or implementation of innovations that will enable improvement. Therefore, we developed a local project that would be implemented in all six integrated care boards (ICBs) of the West Midlands from January 2023 to March 2024.
The HF project has four specific aims. Firstly, it seeks to enhance the detection of patients with HF and ensure timely diagnosis through Natriuretic Peptide tests and echocardiograms in primary care.
Secondly, it aims to improve the quality of GP patient registers in primary care to ensure appropriate coding of patients with HF, whether with reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF).
Thirdly, the project also aims to guarantee that patients with HFrEF receive a 12-monthly review and optimisation of their therapy to prevent avoidable hospital admissions.
Lastly, it seeks to ensure that patients with HFpEF receive optimal management of their co-morbidities
By working in collaboration with the regional cardiac network the project provided regional meetings for HF teams to share and learn and surveyed all the regions heart services to provide a landscape review. This helped embed HF champions into each ICS and targeted primary care networks (PCNs) in relation to health inequalities and heart failure HF prevalence.
The work also supported the workforce of the future by offering upskilling workshops to raise awareness of HF and encouraged the primary care workforce to undertake quality improvements at both PCN and practice levels.
To improve health and wealth, the project delivered evidenced based interventions, through a specialised toolkit aimed at primary care to aid quality improvement projects. The HF champions targeted PCNs in relation to heath inequalities and HF prevalence.
Examples of good practice were identified and case studies produced to aid spread and adoptionof improved HF care.
The HF project has resulted in 46% of PCNs committing to enhancing HF care through engaged champions, dedicated to undertaking improvement initiatives.
Furthermore, 22% of PCNs have embraced our tailored resources for quality enhancement projects. Participating practices have contributed eight insightful case studies, facilitating knowledge dissemination and adoption.
Additionally, eight HF upskilling workshops, attended by 216 individuals, were conducted across the ICB. Some PCN pharmacists have shadowed HF champions, subsequently establishing HF clinics within their PCNs.
A comprehensive toolkit has been developed and shared to support these endeavours. Moreover, a State of the Region report was produced following a comprehensive survey of all HF services, while two regional workshops, in collaboration with the cardiac network, were convened.
ADHD
Attention Deficit Hyperactivity Disorder (ADHD) is a treatable disorder that affects around 5% of school-aged children worldwide. If left undiagnosed or untreated, ADHD can have significant impacts on personal development, academic outcomes, and family interactions. However, the process for diagnosing ADHD takes on average 18 months for children in the UK.
To establish a diagnosis a multi-step process is often used. This involves several appointments and assessments through clinical judgement, informed by subjective reports from parents, teachers, and patient observation, which raise the barrier to treatment access. The volume of activity involved in diagnosis is estimated to cost the NHS £23 million per year. The West Midlands ADHD project provided funding to four hospital trusts in the region to support the adoption of QbTest, which accelerates the diagnosis of ADHD.
The ADHD project set out to accelerate the process of diagnosis of patients with ADHD across four West Midlands trusts, by funding and overseeing the implementation of QbTest. The long-term goal is to create a more sustainable ADHD diagnosis service for the future.
QbTest is an objective, computer-based assessment that supports the ADHD diagnostic pathway, developed by QbTech Ltd. The QbTest assesses a patient’s attention, impulsivity, and motor activity in just 15 minutes. When integrated into ADHD pathways it helps speed up diagnosis and therefore reduces the number of appointments and resources needed.
Health Innovation West Midlands (HIWM) funding supported the four trusts with the implementation of the QbTest, by enabling the sourcing of testing equipment, such as an infrared camera, a headband with an infrared marker, and a responder button.
During the QbTest, several symbols appear on the computer screen and the patient must push the responder button when a particular symbol is shown. The test results are then compiled into a report and compared with data from other people of the same sex and age who have not received an ADHD diagnosis.
These results are used in combination with other ADHD assessment tools to aid clinical judgement. After the test, the results are entered into the child’s record, with a health professional then submitting a referral to paediatricians, along with other documentation from home and school, to support in achieving an ADHD diagnosis.
Progress at each trust was demonstrated via:
- The numbers of staff completing the QbTest training
- The numbers of QbTests conducted
- Completion and submission of quarterly reports to HIWM to understand qualitative progress, successes and barriers
Since its implementation in Q1 of 2023, all four trusts involved in this project successfully adopted QbTesting into their patient pathways to help diagnose ADHD. 722 patients were tested across the trusts, helping surpass the self-assigned target of 288 tests by the end of Q4.
67 staff members also received training to support the new processes and pathways put in place around QbTesting. The project is now complete and exceeded the agreed targets for the 23/24 financial year.
In one trust, offering QbTests with initial appointments after triage, avoided the duplication of administration time. Another trust was able to offer shorter appointment times with senior nurses, and able to assign responsibility for school observations from a senior staff member, to junior staff, helped by the QbTest providing an objective measure in the pathway, bringing efficiency and cost savings.
The individual case studies in this report reflect the organisation’s priorities, which are aligned with the National Health Innovation Network, as well as the needs of our local system. They showcase our impact across our areas of focus from April 2023 – March 2024.
What’s next?
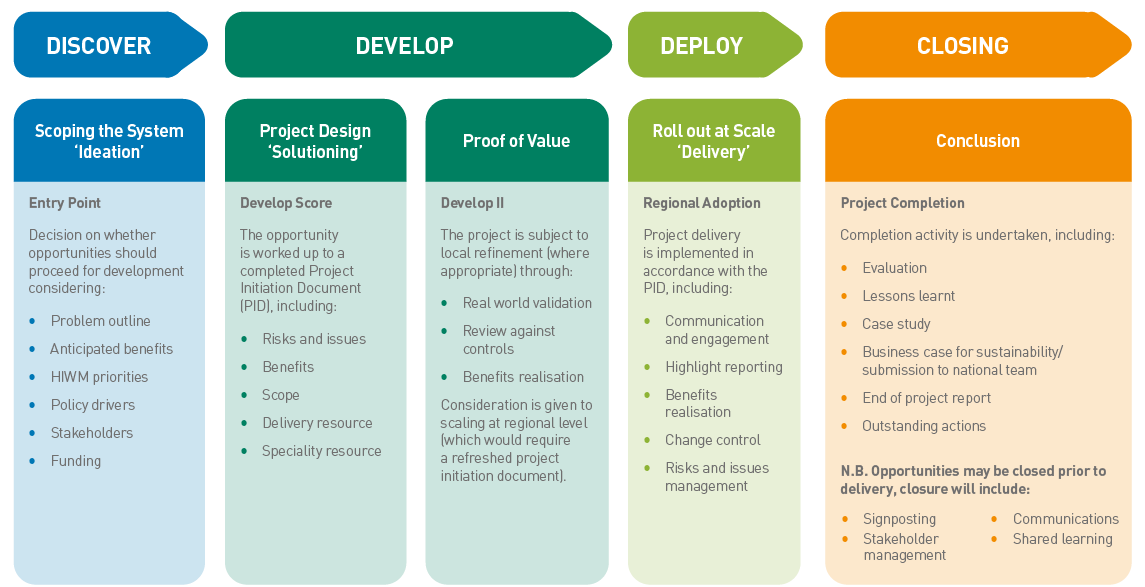
In January 2024, we introduced the pipeline model, taking programmes through a series of gateways:
Discover
Scoping the System
‘Ideation’
Develop
Project Design, ‘Solutioning’
& Proof of Value
Deploy
Roll out at Scale
‘Delivery’
137 programmes are already going through the pipeline and we expect our
Impact Report next year to be much richer with innovations.
Sign up for updates
Sign up to our newsletter for the latest updates and news from Health Innovation West Midlands.